A rural calling: Anya Cope with LMU’s DeBusk College of Osteopathic Medicine has dedicated her career to bringing and retaining more healthcare practitioners in rural communities
Published 11:09 am Friday, June 30, 2023

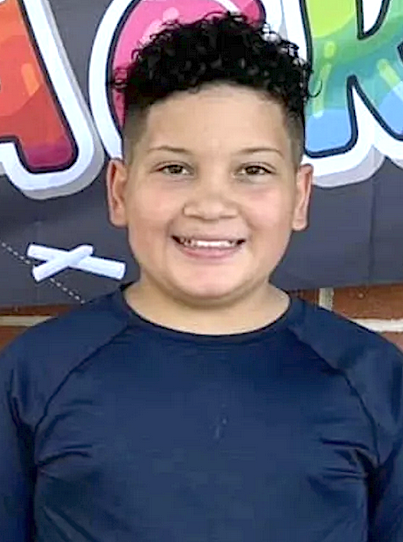
- Anya Cope says that in recruiting students, she’s looking for “someone who is adaptable. Someone who, despite facing adversity, has been able to keep going. Someone who has shown a commitment to medicine, and a passion for medicine.” Photo submitted
|
Getting your Trinity Audio player ready...
|
BY TAYLOR SISK
The Daily Yonder
Cassi Jones’s first impression of Anya Cope when the two met in med school? “Go-getter.” Nothing in the past 17 years has dissuaded her from that assessment. “She’s a fixer,” Jones said. “A doer.”
Today, as associate dean of clinical affairs and an assistant professor of internal medicine at Lincoln Memorial University’s DeBusk College of Osteopathic Medicine, Cope is putting that drive to great use. By living example and through her instruction, she’s demonstrating how to excel in a demanding field when the odds appear to be against you.
Cope was born in rural Southwest Virginia, in the town of Dryden (population 878), an hour’s drive northeast of the DeBusk campus in Harrogate, Tennessee. Her dad mined coal for 25 years, was laid off, then worked a variety of jobs; her mom worked for a power company.
It was in sixth grade that Cope set her mind to becoming a doctor.
“The book fair changed my life,” she said. She discovered a novella by Lurlene McDaniel called Six Months to Live. It’s about a little girl named Dawn Rochelle who’s diagnosed with cancer, and the message Cope took from it was that the way a healthcare provider interacts with a patient makes a world of difference. Kindness matters. She felt called to be that provider.
Cope graduated from high school in 2000. It was, she says, a “weird time” in the mountains of rural Southwest Virginia: The overprescription of opioids had taken deep root, across generations. She’s thankful today for a 9 o’clock curfew.
She considers her education to have been sufficient; she was prepared to be successful at college. But the family had no real knowledge of or resources for board prep courses. Her MCAT score, she says, wouldn’t get her into med school today.
Cope believes schools too often put too much emphasis on standardized testing. “There’s so much more than a number.” She urges administrators to look beyond that number. It tells you nothing about a potential student’s determination, their passion for healing.
For several years, she volunteered at Eagle Mount, a camp for kids with cancer in Bozeman, Montana: “And it was wonderful, and it was heartbreaking, all at the same time, because some kids didn’t come back to camp, because they lost their battle with cancer.”
The experience reinforced what she’d learned from McDaniel’s book. “My time volunteering with Eagle Mount really taught me about empathy and compassion for those around me and about cherishing every day you’re given.”
She decided against pediatric oncology, choosing osteopathic medicine. Osteopathy is a patient-centered, whole-person approach to health care. “It’s believing that the body, mind, and spirit are all connected,” Cope explained. “They have to be working together to achieve good health.” It’s about listening to and partnering with your patient.
Cope practiced in the region for several years before taking the position at Lincoln Memorial.
“I was worried about stepping away from clinical practice,” she said. “I felt, like most physicians do, that nobody takes care of your patients as well as you do. I was talking to my mom about it, and she said, ‘Anya, I know you think you’re the only person who can take care of your patients. But think of it like this: Instead of one person taking care of your patients, you’re teaching 243 people to take care of them just like you do.’”
The DeBusk College of Osteopathic Medicine places emphasis on recruiting students from the region, teaching them in the region, and finding residency opportunities for them here – “And then, hopefully, they’re going to treat my family,” Cope said.
The admissions office has its incentives; Cope supplements those efforts – for example, by visiting the University of Virginia’s College at Wise, where she earned her undergraduate degree, to talk with students. “I’ve been there in the classroom where I took organic chemistry from Dr. Margie Tucker and told them, ‘I was in your shoes. Literally, I sat in that seat,’” she recalled.
The outreach, she believes, must start early.
“Too many kids in this region think their only options are coal mining, teaching, and nursing – all of which are commendable careers – or illegal drug dealing,” she said. “You can’t be it if you don’t see it. We need to show them there are other options – that there are people from here who are succeeding in all kinds of fields. And it has to be before high school.”
Toward that end, the college is setting up camps for pre-K through eighth-grade students that will offer opportunities to study STEM topics, explore career choices, and gain skills necessary to be successful in those fields.
Among Cope’s primary duties as assistant dean of clinical affairs is ensuring there are enough sites for DeBusk’s third- and fourth-year students to complete their clinical training and that each student is getting what they need from those experiences. Students complete four-week rotations with multiple physicians to gain clinical knowledge and skills while deciding on their specialty. The college currently has 43 core rotation sites in 11 states.
Another role is establishing graduate medical education programs, which requires building relationships with hospital staff. “My job is all about relationships,” Cope said.
Most fundamentally, it’s about nurturing relationships with students. The type of student she’s looking for is “someone who is adaptable. Someone who, despite facing adversity, has been able to keep going. Someone who has shown a commitment to medicine, and a passion for medicine.”
“Of course,” she added, “we want someone who is drawn to Appalachia and to rural medicine. But I think that even those who have not had the experience of rural medicine, once they get here, we can convince them.”
Research substantiates this. A 2021 Journal of Graduate Medical Education study found that “Physicians often practice within 100 miles of where they completed residency” and “Training residents where they are needed in practice is one promising strategy to increase the supply of rural physicians.”
Why osteopathy? “I think for a lot of different reasons,” Cope said. “I think it’s just the ability to slow down for a minute and listen to my patient and consider all possibilities. Now, don’t get me wrong: I think osteopaths and allopaths have more in common than we have differences. There are amazing allopathic physicians who believe in the holistic approach.”
Osteopaths, though, are “taught from day one that the body can heal itself when given the right conditions and that we can really affect healing based on how we approach the patient. I think those are really good skills to impart to students from the beginning.”
Personally, she’s driven to underscore for those from rural communities that “you can be just as good as any others – and maybe better because of the resistance you’ve had to fight against. It’s like cross-training: fighting against resistance makes you stronger.”
“She’s a true believer; she believes in what she’s doing,” Christopher Loyke, dean and chief academic officer of the College of Osteopathy, said. “She really is driven.”
Cope’s med school classmate Cassi Jones is now her colleague, serving as DeBusk’s director of clinical affairs and an assistant professor of internal medicine. She too is Appalachian bred – central Kentucky – and believes it serves her and Cope well in their joint mission.
“We know the issues this region faces,” Jones said, “And we also have experience with the biases [of outside observers].”
She admires how Cope prepares her students to practice in marginalized communities. “One of the things that I think everybody can learn by working with her and just seeing how she operates,” Jones said, “She never assumes.” According to Jones, Cope never assumes she knows the reality of things before asking those questions. “She always asks the right questions. And that’s how we really start making a difference in rural health care.”
Nancy Myers is a family friend who at the time Cope was applying to med schools worked for the Area Health Education Center program. She helped guide Cope through that arduous process.
“‘Determined’ is the best word to describe Dr. Cope, determined to help others,” said Myers, who now serves as DeBusk’s director of clinical partnerships. “I once said that if Anya Cope decided that she could best serve by being president of the United States, they may as well clear out the Rose Garden for her farm animals, because she is coming.”